Sickle cell disease
Highlights
What is Sickle Cell Disease?
Sickle cell disease is an inherited blood disorder in which the body produces abnormally shaped red blood cells. In sickle cell disease, the hemoglobin in red blood cells clumps together. This causes red blood cells to become stiff and C-shaped. These sickle cells block blood and oxygen flow in the body. Sickle cells break down more rapidly than normal red blood cells, which can result in anemia.
What Causes Sickle Cell Disease?
Sickle cell disease is a genetic disorder. People who have sickle cell disease are born with two sickle cell genes, one from each parent. If one normal hemoglobin gene and one sickle cell gene are inherited, a person will have sickle cell trait. People who have sickle cell trait do not develop sickle cell disease, but they are “carriers” who can pass the abnormal gene on to their children.
Complications of Sickle Cell Disease
Sickle cell disease can block the flow of blood in arteries in many parts of the body, causing many complications. The hallmark of sickle cell disease is the sickle cell crisis, which causes sudden attacks of severe pain. Acute chest syndrome, which is triggered by infection or blockage of blood vessels in the lungs, is also a common and serious occurrence. Other medical complications include:
- Infections
- Pulmonary hypertension (increased pressure in the arteries of the lungs)
- Stroke
- Anemia
- Kidney problems
- Priapism (prolonged and painful erections)
- Liver problems
- Gallbladder disease
- Spleen damage
- Bone and joint problems
- Leg sores and ulcers
- Eye damage in the retina
Introduction
Sickle cell disease (also called sickle cell anemia) is an inherited blood disorder that affects red blood cells. The sickle cell gene causes the body to produce abnormal hemoglobin. In sickle cell disease, the hemoglobin clumps together, causing red blood cells to become stiff and develop a C-shaped (“sickle”) form. These sickled red blood cells can block blood vessels, reducing blood flow in many parts of the body. This process results in tissue and organ damage.
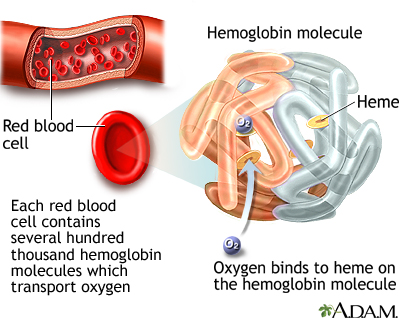
Hemoglobin and Iron
Each red blood cell contains about 280 million hemoglobin molecules. Hemoglobin is the most important component of red blood cells. It is composed of protein (globulin) and a molecule (heme), which binds to iron.
In the lungs, the heme component takes up oxygen and releases carbon dioxide. The red blood cells carry the oxygen to the body's tissues, where the hemoglobin releases the oxygen in exchange for carbon dioxide, and the cycle repeats. The oxygen is essential for all cells in the body to function.
Sickle cell disease reduces or denies adequate oxygen to many parts of the body. This contributes to the severe pain experienced as a sickle cell crisis and both short- and long-term organ damage.
Causes
Sickle Cell Disease and Hemoglobin
Sickle cell disease occurs from genetic changes that cause abnormalities in hemoglobin molecules:
- Hemoglobin A (HbA). HbA is the hemoglobin molecule found in normal red blood cells during childhood and adulthood. People who do not have sickle cell disease generally have this type of hemoglobin in their blood cells.
- Hemoglobin S (HbS). HbS (S is for sickle) is the abnormal variant of hemoglobin A, which occurs in sickle-red blood cells and is the primary characteristic of the disease. The difference between hemoglobin A (HbA) and hemoglobin S (HbS) is that only one protein out of about 300 are common to both. This protein lies along an amino-acid chain called beta-globin, where even a tiny abnormality has disastrous consequences.
The Sickle Cell Disease Process
The symptoms and problems of sickle cell disease are a result of the hemoglobin S (HbS) molecule:
- When the sickle hemoglobin molecule loses its oxygen, it forms rigid rods called polymers that change the red blood cells into a sickle or crescent shape.
- These sickle-shaped cells stick to the walls and cannot squeeze through the capillaries. Blood flow through tiny blood vessels becomes slowed or stopped in many parts of the body. This deprives tissues and organs of oxygen.
- When this blood flow slows or stops suddenly in a certain part of the body, the decrease in oxygen (hypoxia) can cause severe pain (the sickle cell crisis). Over time, it leads to gradual destruction in organs and tissues throughout the body.
- The higher the concentration of sickle hemoglobin and the more acidic the environment, the faster the sickle cell process is.
- When blood cells dry out (dehydrate), the density of hemoglobin S within the cell increases, thereby speeding the sickling process.
- Sickle cells also have a shorter life span (10 - 20 days) than normal red blood cells (90 - 120 days). Every day the body produces new red blood cells to replace old ones, but sickle cells become destroyed so fast that the body cannot keep up. The red blood cell count drops, which results in anemia. This gives sickle cell disease its more common name, sickle cell anemia.
Risk Factors
The sickle cell gene for hemoglobin S (HbS) is the most common inherited blood condition in the United States. About 70,000 - 100,000 Americans -- mostly African-Americans -- have sickle cell disease. About 2 million Americans have sickle cell trait.
Sickle cell disease is inherited. People at risk for inheriting the gene for sickle cell descend from people who are or were originally from Africa or parts of India and the Mediterranean. The sickle cell gene also occurs in people from South and Central America, the Caribbean, and the Middle East. The high prevalence of the sickle cell gene in these regions of the world is due to the sickle cell's ability to make red blood cells resistant to the malaria parasite.
People inherit a pair of genes that regulate hemoglobin, with one gene coming from each parent:
- If one normal hemoglobin gene and one sickle cell gene are inherited, a person will have sickle cell trait. People who have sickle cell trait are protected from malaria and do not develop sickle cell disease, but they are “carriers” who can pass the abnormal gene on to their children. In general, most people with sickle cell trait are healthy, although some individuals may face kidney complications and other health problems.
- If two sickle genes are inherited, a person will have sickle cell disease.
Risk of Inheritance
The risk of a child inheriting sickle cell disease or sickle cell trait is as follows:
- If both parents have sickle cell trait (each have one normal hemoglobin gene and one sickle cell gene), the child has a 50% chance of inheriting sickle cell trait (one normal gene, one sickle cell gene), 25% chance of inheriting sickle cell disease (two sickle cell genes), and 25% chance of not inheriting either the trait or the disease (two normal genes).
- If one parent has sickle cell trait (one normal gene and one sickle cell gene) and the other parent has two normal hemoglobin genes, the child has a 50% chance of inheriting sickle cell trait (one normal gene and one sickle cell gene) and a 50% of inheriting neither the trait nor the disease (two normal genes). The child is not at risk of inheriting sickle cell disease.
- If one parent has sickle cell disease (two sickle cell genes) and the other parent has sickle cell trait (one normal gene, one sickle cell gene), the child has a 50% chance of inheriting sickle cell trait and a 50% chance of inheriting sickle cell disease.
- If one parent has sickle cell disease and the other parent has two normal hemoglobin genes, the child has a 100% chance of inheriting sickle cell trait, but not the disease.
- If both parents have sickle cell disease, the child has a 100% chance of inheriting the disease.
Symptoms
General Symptoms in Infants. In infants, symptoms do not usually appear until late in the baby's first year. Most commonly, they include:
- Fever
- Swelling of the hands and feet
- Pain in the chest, abdomen, limbs, and joints
- Nosebleeds and frequent upper respiratory infections
General Symptoms in Children. Pain is the most common complaint. It can be acute and severe or chronic, usually from orthopedic problems in the legs and low back. Other symptoms include:
- Fatigue and shortness of breath (signs of anemia)
- Irritability
- Jaundice (yellowish discoloration of the skin and eyes)
Additional Symptoms in Adolescence or Adulthood. Symptoms from childhood continue in adolescence and adulthood. In addition, patients may have:
- Delayed puberty (in young teenagers)
- Severe joint pain
- Progressive anemia
- Leg sores
- Gum disease
- Vision problems
Sickle Cell Crisis
Sickle cell crises are episodes of pain that occur with varying frequency and severity in different patients and are usually followed by periods of remission. Severe sickle cell pain has been described as being equivalent to cancer pain and more severe than postsurgical pain. It most commonly occurs in the lower back, leg, abdomen, and chest, usually in two or more locations. Episodes usually recur in the same areas. (See "Pain and Acute Sickle Cell Crisis" in Complications section of this report.)
Diagnosis
Blood tests can determine whether an individual has sickle cell trait or sickle cell disease.
Screening Tests for Newborns
In the United States, hospitals routinely screen newborn babies for sickle cell disease. To perform the test, a blood sample is taken from the baby's heel using a simple needle prick. Early detection of sickle cell disease can help reduce the risk of life-threatening infections and increase the odds for survival. Babies who are diagnosed with sickle cell disease are given daily antibiotics to help prevent infections.
Prenatal diagnosis is also possible through amniocentesis. The amniotic fluid is tested for the presence of the sickle cell gene.
Diagnostic Tests for Stroke
Unfortunately, no tests can definitely determine which children are at highest risk for a stroke and, therefore, would be candidates for ongoing blood transfusions. The following are diagnostic tools currently used or under investigation:
- Transcranial Doppler (TCD) ultrasonography measures the speed of blood flow in the brain. It can be used for identifying children at risk for stroke. However, high-risk children are still vulnerable to stroke even if the TCD screening diagnoses normal blood flow velocities.
- Magnetic resonance imaging (MRI) can detect small blockages in blood vessels and may help confirm high risk in patients identified by TCD ultrasound.
- Angiography is an invasive diagnostic technique useful for detecting aneurysms. (An aneurysm is a bulging in the blood vessel wall, which can result in stroke if it bursts in the brain.)
- Genetic markers may eventually be used to help identify sickle cell patients at higher risk for stroke.
Prognosis
New and aggressive treatments for sickle cell disease are prolonging life and improving its quality. As recently as 1973, the average lifespan for people with sickle cell disease was only 14 years. Today, life expectancy for these patients can reach 50 years and beyond. Women with sickle cell usually live longer than their male counterparts.
The damage of sickle cell disease occurs because the logjam that sickle cells cause in the capillaries slows the flow of blood and reduces the supply of oxygen to various tissues. Not only does pain occur when body tissues are damaged by lack of oxygen, but serious and even life-threatening complications can result from severe or prolonged oxygen deprivation. Sickle cell disease is referred to in some African languages as "a state of suffering," but the disease has a wide spectrum of effects, which vary from patient to patient. In some people, the disease may trigger frequent and very painful sickle cell crises that require hospitalization. In others, it may cause less frequent and milder attacks.
Children with sickle cell disease are very susceptible to infections, mostly because their damaged spleens are unable to protect the body from bacteria. Signs of impaired lung function may occur even in very early years. Because children with sickle cell disease are living longer, older patients are now facing medical problems related to the long-term adverse effects of the disease process. The most serious dangers are acute chest syndrome, long-term damage to major organs, stroke, and complications during pregnancy such as high blood pressure in the mother and low birth weight in the infant.
Complications
There is still no cure for sickle cell disease other than experimental transplantation procedures, but treatments for complications of sickle cell have prolonged the lives of many patients who are now living into adulthood.
Pain and Acute Sickle Cell Crisis
The hallmark of sickle cell disease is the sickle cell crisis (sometimes known as a vaso-occlusive crisis), which is an episode of pain. It is the most common reason for hospitalization in sickle cell disease. The pattern may occur as follows:
- In general, the risk for a sickle cell crisis is increased by any activity that boosts the body's requirement for oxygen such as illness, physical stress, or being at high altitudes. In more than half of episodes, however, the trigger is unknown.
- Episodes typically begin at night and last 3 - 14 days, accelerating to a peak over several days and then declining.
- The pain is typically described as sharp, intense, and throbbing. Severe sickle cell pain has been described as being equivalent to cancer pain and more severe than postsurgical pain. Shortness of breath is common.
- Pain most commonly occurs in the lower back, leg, hip, abdomen, or chest, usually in two or more locations. Episodes usually recur in the same areas. Pain in the bones (usually occurring symmetrically on both sides) is common because blood obstruction can directly damage bone and because bone marrow is where red blood cells are manufactured.
- The liver or spleen may become enlarged, causing pain in the upper right or upper left sides of the abdomen. Liver involvement may also cause nausea, low-grade fever, and increasing jaundice.
- Males of any age may have prolonged, often painful erections, a condition called priapism.
Episodes cannot be predicted, and they vary widely among different individuals. Episodes sometimes become less frequent with increasing age. Generally, people can resume a relatively normal life between crises. Most patients are pain-free between episodes although pain can be chronic in some cases.
Acute Chest Syndrome (ACS)
Acute chest syndrome (ACS) occurs when the lung tissues are deprived of oxygen during a crisis. It can be very painful, dangerous, and even life threatening. It is a leading cause of illness among sickle cell patients and is the most common condition at the time of death. At least one whole segment of a lung is involved, and the following symptoms may be present:
- Fever of 101.3 °F degrees (38.5 °C) or above
- Rapid or labored breathing
- Wheezing or cough
- Acute chest pain
Pain often lasts for several days. In about half of patients, severe pain develops about 2 - 3 days before there are any signs of lung or chest abnormalities. Acute chest syndrome is often accompanied by infections in the lungs, which can be caused by viruses, bacteria, or fungi. Pneumonia is often present. A dull, aching pain usually follows, which most often ends after several weeks, although it may persist between crises.
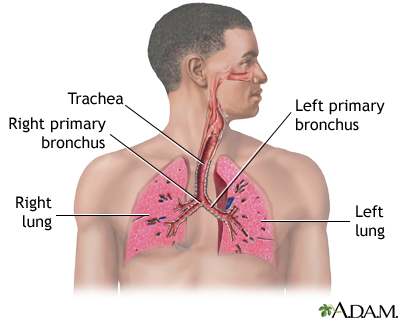
Causes of Acute Chest Syndrome. Primary causes of acute chest syndrome include:
- Infection. Infection from viruses or small atypical organisms (Chlamydia and Mycoplasma) is the most common cause of the oxygen deprivation that leads to acute chest syndrome.
- Blockage of blood vessels. Blockage in the blood vessels that cuts off oxygen in the lungs is another important cause of acute chest syndrome. Blockage may be produced by blood clots or fat embolisms. (Fat embolisms are particles formed from fatty tissue in the bone marrow that enter and travel through the blood vessels.)
- Asthma. Asthma can increase the frequency and pain of acute chest syndrome episodes in children. Children with sickle-cell disease who have frequent acute chest syndrome attacks should be evaluated for asthma.
Some cases of acute chest syndrome may result from treatments of the crisis, including from administration of opioid pain killers (which can reduce breathing and oxygen uptake) or excessive use of intravenous fluids. Other lung diseases may also trigger ACS.
Severity of Acute Chest Syndrome. The mortality rates for ACS are around 2% in children and 4% in adults. The syndrome and its long-term complications are the major causes of death in older patients. The longer a patient survives, the more repetitive sickle cell crises damage the chest and lungs.
The following destructive effects can occur:
- Damage in the chest area from recurrent episodes increases susceptibility to infections, even those caused by organisms that are ordinarily not harmful.
- Lung damage over time can lead to obstruction in the airways in lungs, causing asthma-like conditions.
Infections
Infections are common and an important cause of severe complications. Before early screening for sickle cell disease and the use of preventive antibiotics in children, 35% of infants with sickle cell died from infections. Fortunately, with screening tests for sickle cell now required for newborns, and with the use of preventive antibiotics and immunizations in babies who are born with the disease, the mortality rate has dropped significantly.
Infections in Infants and Toddlers with Sickle Cell Disease. The most common organisms causing infection in children with sickle cell disease include:
- Streptococcus pneumoniae (can cause pneumonia, blood infections, or meningitis)
- Haemophilus influenza (also a cause of pneumonia, blood infections, and meningitis)
Such infections pose a serious threat to infants and very young children with sickle cell disease. They can progress to fatal pneumonia with devastating speed in infants, and death can occur only a few hours after onset of fever. The risk for pneumococcal meningitis, a dangerous infection of the central nervous system, is also significant.
Infections in Children and Adults. Infections are also common in older children and adults with sickle cell disease, particularly respiratory infections such as pneumonia, kidney infections, and osteomyelitis, a serious infection in the bone. (The organisms causing them, however, tend to differ from those in young children.) Infection-causing organisms include:
- Chlamydia pneumoniae and Mycoplasma pneumoniae. These are the important infections in acute chest syndrome (see above).
- Gram-negative bacteria. This group of bacteria mostly infects hospitalized patients and can cause serious pneumonias and other infections.
Pulmonary Hypertension
About 30% of patients with sickle cell disease have pulmonary hypertension. Pulmonary hypertension is a serious and potentially deadly condition that develops when pressure in the arteries of the lungs increases. It is an often unrecognized complication and a significant cause of death in sickle cell disease. Many doctors recommend that all adults with sickle cell disease have echocardiographic testing to identify if they are at risk for pulmonary hypertension and need treatment.
The primary symptom of pulmonary hypertension is shortness of breath, which is often severe. Pulmonary hypertension can be very serious and life threatening in the short- and long-term. If pulmonary hypertension develops suddenly it can cause respiratory failure, which is life threatening. Over time, pulmonary hypertension may cause a condition called cor pulmonale, in which the right side of the heart increases in size. In some cases, this enlargement can lead to heart failure.
Stroke
After acute chest syndrome, stroke is the most common killer of patients with sickle cell disease who are older than 3 years old. Between 8 - 10% of patients suffer strokes, typically at about age 7. Patients may also suffer small strokes that may not be immediately noticeable. However, patients who have many of these small strokes may over time start behaving differently or have worsening mental functioning.
Strokes are usually caused by blockages of vessels carrying oxygen to the brain. Patients with sickle cell disease are also at high risk for stokes caused by aneurysm, a weakened blood vessel wall that can rupture and hemorrhage. Multiple aneurysms are common in sickle cell patients, but they are often located where they cannot be treated surgically.
Anemia
Anemia is a significant characteristic in sickle cell disease (which is why the disease is commonly referred to as sickle cell anemia).
Severe worsening of anemia. Children, adolescents, and possibly young adults may experience what is called splenic sequestration. This happens when a large number of sickled red blood cells collect in the patient's spleen. Symptoms may include pain in the right abdomen below the ribs and a large mass (the swollen spleen) may be felt.
Chronic Anemia. Because of the short lifespan of the sickle red blood cells, the body is often unable to replace red blood cells as quickly as they are destroyed. This causes a particular form of anemia called hemolytic anemia. Most patients with sickle cell disease have hemoglobin levels of about 8 g/dL, much lower than healthy people. Chronic anemia reduces oxygen levels and increases the demand on the heart to pump more oxygen-bearing blood through the body. Eventually, this can cause the heart to become dangerously enlarged, with an increased risk for heart attack and heart failure.
Sometimes patients may have what is called an aplastic crisis. This happens when the cells in the bone marrow that are normally trying to make new red blood cells suddenly stop working. This sudden stopping is often triggered by a virus called human parvovirus B19.
Kidney Problems
The kidneys are particularly susceptible to damage from the sickling process. Persistent injury can cause a number of kidney disorders, including infection. Problems with urination are very common, particularly uncontrolled urination during sleep. Patients may have blood in the urine, although this is usually mild and painless and resolves without damaging consequences. Kidney failure is a major danger in older patients and accounts for 10 - 15% of deaths in sickle cell patients. Renal medullary carcinoma is an aggressive, rapidly destructive tumor in the kidney that is rare but can occur in association with sickle cell disease.
Priapism
About 40% of males, including children, with sickle cell disease suffer from priapism. Priapism causes prolonged and painful erections that can last from several hours to days. If priapism is not treated, permanent partial or complete erectile dysfunction can occur.
Liver Problems
Enlargement of the liver occurs in over half of sickle cell patients, and acute liver damage occurs in up to 10% of hospitalized patients. Because sickle cell patients often need transfusions, they are at higher risk for viral hepatitis, an infection of the liver. This risk, however, has decreased since screening procedures for donated blood have been implemented.
Gallbladder Disease
About 30% of children with sickle cell disease have gallstones, and by age 30, 70% of patients have them. In most cases, gallstones do not cause symptoms for years. When symptoms develop, patients may feel overly full after meals, have pain in the upper right quadrant of the abdomen, or have nausea and vomiting. Acute attacks can be confused with a sickle cell crisis in the liver. Ultrasound is usually used to confirm a diagnosis of gallstones. If the patient does not have symptoms, no treatment is usually necessary. If there is recurrent or severe pain from gallstones, the gallbladder may need to be removed. Minimally invasive procedures (using laparoscopy) reduce possible complications. [For more information, see In-Depth Report #10: Gallstones.]
Spleen Damage
The spleen of most adults with sickle cell anemia is nonfunctional due to recurrent episodes of oxygen deprivation that eventually destroy it. Injury to spleen increases the risk for serious infection. Acute splenic sequestration crisis (sudden spleen enlargement) can occur when the spleen suddenly becomes enlarged from trapped blood.
Bone and Joint Problems
In some children with sickle cell disease, excessive production of blood cells in the bone marrow causes bones to grow abnormally, resulting in long legs and arms or misshapen skulls. Sickling that blocks oxygen to the bone can also cause bone loss and pain. Sickling that affects the hands and feet of children causes a painful condition called hand-foot syndrome. A condition called avascular necrosis of the hip occurs in about half of adult sickle cell patients when oxygen deprivation causes tissue death in the bone. Eventually adult patients may need surgery to remove diseased and dead bone tissue. Patients with severe cases may need joint replacement.
Leg Sores and Ulcers
Leg sores and ulcers may occur. They usually affect patients older than 10 years.
Eye Problems
Sickle cell disease can damage blood vessels in the eye and cause scarring and detachment of the retina, which can lead to blindness.
Pregnancy and Sickle Cell Disease
Women with sickle cell disease who become pregnant are at higher risk for complications such as miscarriage and premature birth, and their babies may have low birth weight. Sickle cell disease symptoms often worsen during pregnancy and pain crises become more frequent. However, with careful prenatal care and monitoring, serious problems can be avoided. Maternal mortality rates have dropped significantly over the past decades. Most women with sickle cell disease can now anticipate favorable pregnancy outcomes.
Other Medical Complications
Older children and adult patients with sickle cell are subject to other medical problems, including impaired physical development and gum disease. In severe cases, sickle cell disease can cause multiple organ failure.
Treatment
Treatment goals for sickle cell disease aim to relieve pain, prevent infections, and manage complications. [For specific information on complications, see Treatment of Complications section in this report.] Patients should seek care from a doctor who specializes in blood disorders (hematologist) or a clinic that is experienced in treating sickle cell disease.
Bone marrow transplantation is the only potential cure, but it is used in only a small number of cases as few patients are able to find donors who are suitable genetic matches. Blood transfusions are given to prevent worsening anemia and prevent stroke.
Drug treatments for sickle cell disease include:
- Antibiotics, usually penicillin, are commonly given to infants and young children, as well as adults, to help prevent infections.
- Pain relief medications ranging from nonprescription nonsteroidal anti-inflammatory drugs (NSAIDs) to opiods are given to control pain.
- Hydroxyurea (Droxia) is prescribed for patients with moderate-to-severe sickle cell disease to help reduce the frequency of pain episodes and acute chest syndrome.
Hydroxyurea
HbF, also called fetal hemoglobin, is the form of hemoglobin present in the fetus and young infants. Most HbF disappears early in childhood, although some HbF may persist. Fetal hemoglobin is able to block the sickling action of red blood cells. Because of this, infants with sickle cell disease do not develop symptoms of the illness until HbF levels have dropped. Adults who have sickle cell disease but still retain high levels of hemoglobin F generally have mild disease.
Hydroxyurea (Droxia) is a drug that reduces the severity of sickle cell disease by stimulating production of HbF. It is currently the only drug in general use to prevent acute sickle cell crises.
Hydroxyurea is recommended as frontline therapy to treat adults and adolescents with moderate-to-severe recurrent pain (occurring three or more times a year). Hydroxyurea reduces the frequency of acute pain crises and episodes of acute chest syndrome. It is taken daily by mouth. Hydroxyurea can be taken indefinitely and the benefits appear to be long-lasting.
Hydroxyurea is not a cure-all. Not all patients respond to hydroxyurea, and the best candidates for the treatment are not yet clear. Many patients who could benefit from this medication are not receiving it. Hydroxyurea is still being investigated for younger patients. To date, the response to the drug in children with sickle cell disease is similar to the response in adults, and few severe adverse effects are being reported. Recent research also suggests that hydroxyurea is safe for infants.
Side effects include constipation, nausea, drowsiness, hair loss, and inflammation of the mouth. More severe side effects include reduction of white blood cells (neutropenia) and the cells responsible for normal blood clotting (thrombocytopenia). Hydroxyurea should not be taken by women because it can cause birth defects. There have been concerns that long-term use of hydroxyurea may increase the risk of developing leukemia, but the significance of this risk remains unclear. Still, for many patients the risks of untreated sickle cell disease may outweigh the risks of hydroxyurea’s side effects.
Patients should handle hydroxyurea with care and wash their hands before and after touching the bottle or capsules. Household members who are not taking hydroxyurea (such as caregivers) should wear disposable gloves when handling the medicine or its bottle.
Transfusion
Blood transfusions are often critical for treating sickle cell disease. Transfusions may be used either as treatment for specific episodes or as chronic transfusion therapy to prevent life-threatening complications Ongoing transfusions can also help improve height and weight in children with sickle cell disease. Normal hemoglobin levels for patients with sickle cell disease are around 8 g/dL. Doctors will try to keep the hemoglobin level no higher than 10 g/dL after transfusion.
Episodic Transfusions. Episodic transfusions are needed in the following situations:
- To manage sudden severe events, including acute chest syndrome, stroke, widespread infection (septicemia), and multi-organ failure.
- To manage severe anemia, usually caused by splenic sequestration (dangerously enlarged spleen) or aplasia (halting of red blood cell production, most often caused by parvovirus). Transfusions are generally not necessary for mild or moderate anemia.
- Before major surgeries. Transfusions are generally not required for minor surgeries.
Chronic Transfusions. Chronic (on-going) transfusions are used for:
- Stroke prevention for first or recurrent strokes. Evidence shows that regular (every 3 - 4 weeks) blood transfusions can reduce the risk of a first stroke by 90% in high-risk children. In addition, studies indicate that as many as 90% of patients who have experienced a stroke do not experience another stroke after 5 years of transfusions. The U.S. National Institutes of Health strongly recommends that doctors do not stop regular transfusions for children with sickle cell disease who are at high risk for stroke.
- Pulmonary hypertension and chronic lung disease
- Heart failure
- Chronic kidney failure and severe anemia
- To reduce episodes of pain and acute chest syndrome
Chronic blood transfusions carry their own risks, including iron overload, alloimmunization (an immune response reaction), and exposure to bloodborne microbes. Still, data from large-scale trials suggest that the risks for stroke outweigh the risks associated with transfusions. Researchers are working on ways to reduce the side effects associated with transfusion treatment.
Kinds of Transfusions. Transfusions may be either simple or exchange.
- Simple Transfusion. Simple transfusions involve the infusion of one or two units of donor blood to restore blood volume levels and oxygen flow. It is used for moderately severe anemia, severe fatigue, and nonemergency situations when there is a need for increased oxygen. It is also used for acute chest syndrome.
- Exchange Transfusion. Exchange transfusion involves drawing out the patient's blood while exchanging it for donor red blood cells. Exchange transfusions may be used when there is any evidence that the patient's condition is deteriorating. It prevents stroke and also may be used in patients with severe acute chest syndrome. It reduces the risk of iron overload in patients who require chronic transfusion therapy.
Iron Overload and Chelation Therapy. Iron overload increases risk for damage to the liver, heart, and other organs. A liver biopsy accurately determines whether excess iron levels are present.
Chelation therapy is used to remove excess iron stores in the body. The drug deferoxamine (Desferal) is commonly used during such therapy. Unfortunately, deferoxamine has some severe side effects and must be used with a pump for about 12 hours each day. Many patients do not continue treatment. A newer drug deferasirox (Exjade) is approved for the treatment of transfusion-related iron overload in patients ages 2 and older. It is taken once a day by mouth. Patients mix the pills in liquid and drink the mixture. This new treatment may make chelation therapy much easier and less painful for patients.
Other Complications of Transfusion Therapy.
- Immune reactions. An immune reaction may occur in response to donor blood. In such cases, the patient develops antibodies that target and destroy the transfused cells. This reaction, which can occur 5 - 20 days after transfusion, can result in severe anemia and may be life-threatening in some cases. It can usually be prevented with careful screening and matching of donor blood groups before the transfusion.
- Hyperviscosity. With this condition, a mixture of hemoglobin S and normal hemoglobin causes the blood to become too "thick". The patient is at risk for high blood pressure, altered mental status, and seizures. Careful monitoring can prevent this condition.
- Transmission of viral illness. Before widespread blood screening, transfusions were highly associated with a risk for hepatitis and HIV. This complication has decreased considerably.
Bone Marrow or Stem Cell Transplantation
At this time, the only chance for cure for sickle cell disease is bone marrow or stem cell transplantation. The bone marrow nurtures stem cells, which are early cells that mature into red and white blood cells and platelets. By destroying the sickle cell patient's diseased bone marrow and stem cells and transplanting healthy bone marrow from a genetically-matched donor, normal hemoglobin may be produced.
Bone marrow transplantations have been performed successfully in select children with sickle cell disease. However, due to a lack of available donors and the risks of potential complications, bone marrow transplantations for sickle cell disease are not routinely performed. Complications can include the immune system’s rejection of the transplant (a condition called graft-versus-host-disease) and serious infections. Patients can suffer serious neurological damage if the procedure triggers bleeding in the brain. In general, younger children are considered better candidates for bone marrow transplantation than older children.
Before a bone marrow transplant can be performed, the patient must undergo chemotherapy to completely destroy their own bone marrow. Bone marrow transplantation is considered too risky for adults with sickle cell disease, because they cannot tolerate the chemotherapy regimen as well as children and they tend to have long-term organ damage as a result of the condition.
In 2009, researchers performed a modified type of blood stem-cell transplant that appeared to cure sickle cell disease in 9 of the 10 adults who participated in the clinical trial. The patients ranged from ages 16 - 45, and all had severe sickle cell disease with serious organ complications. In contrast to the procedure performed in children, these patients had only part of their bone marrow replaced. Prior to the transplant, they were treated with low doses of radiation and two drugs (alemtuzumab and sirolimus), which helped suppress their immune systems and prevent rejection. While this procedure is still experimental, it offers hope for elimination of sickle cell disease in adult patients.
Other Investigational Treatments
Nitric Oxide. Nitric oxide is a natural chemical in the body that relaxes smooth muscles and widens blood vessels. Patients with sickle cell disease are deficient in nitric oxide. This lack of nitric oxide constricts blood vessels and causes sickle cell pain. Some studies have indicated that inhaling nitric oxide may slow the disease process and improve symptoms in acute sickle cell crises. Other studies report that nitric oxide is of no benefit. In addition, nitric oxide is difficult to administer. More studies are needed to determine if nitric oxide should have a role in sickle cell therapy. (Nitric oxide is not the same substance as nitrous oxide, the so-called laughing gas used in dentistry.)
Arginine. Arginine is an amino acid involved in producing nitric oxide. Because a lack of arginine may contribute to the development of pulmonary hypertension, (a leading cause of death in patients with sickle cell disease), arginine is being studied as a potential drug treatment. Some research is also being conducted on arginine nutritional supplements. Patients should talk to their doctors before taking these or any other supplements.
Drugs to Prevent Dehydration. Researchers are studying various drugs, as well as mineral supplements such as magnesium pidolate and zinc sulfate, that may help prevent potassium loss and red blood cell dehydration.
Treatment of Complications
Treatment of Pain
The basic objectives for managing a sickle cell crisis are control of pain and rehydration by administration of fluids. Oxygen is typically given for acute chest syndrome. Pain medications can help reduce the severe pain of sickle cell crises. These medications can range from non-prescription pain relievers, such as acetaminophen or nonsteroidal anti-inflammatory drugs, to more powerful narcotics, such as the opioid drug morphine. Corticosteroid drugs may also be prescribed.
All patients should have a treatment plan that helps guide them and their families during a pain episode. Plans should outline which medicines to take and when to seek medical help. Patients and families should learn to recognize symptoms early and begin managing with an appropriate amount of pain medication.
Treatment of Acute Chest Syndrome (ACS)
Acute chest syndrome can be fatal and must be treated immediately. Basic treatments include:
- Supplementary oxygen -- this is critical and life saving.
- Administration of fluids -- overhydration should be avoided to reduce the risk of fluid in the lungs.
- Pain relievers
- Bronchoscopy (a diagnostic procedure involving insertion of a tube into the lower airways) may be needed to identify infection.
Other treatments include:
- High-dose intravenous corticosteroids (usually dexamethasone) may speed recovery from acute chest syndrome and reduce the duration of hospitalization.
- Antibiotics that specifically target the organisms (Chlamydia and Mycoplasma) that commonly trigger acute chest syndrome. Such antibiotics include azithromycin, clarithromycin, levofloxacin, and various tetracyclines (tetracyclines are not used for children).
- Transfusions are important early on for rapid improvement in severe cases, especially if fat embolisms have developed.
Treatment of Infections
Fever in any sickle cell patient should be considered an indication of infection. Temperatures over 101 °F in children warrant a call to the doctor. Adults with sickle cell should call the doctor if they have a have fever over 100 °F and any signs of infection, including chest pain, productive cough, urinary problems, or any other symptoms. Pneumonia is common among patients with sickle cell disease, as are meningitis, influenza, and hepatitis. Bone infections (osteomyelitis) can develop.
When patients with sickle cell develop infections, they are nearly always hospitalized immediately and treated with intravenous or high-dose injections of antibiotics in order to prevent septicemia, the dangerous spread of the infection throughout the body. Antibiotics are also given on an outpatient basis.
It is important for patients with sickle cell disease, especially children, to receive vaccinations to protect against infections. [For more information, see Prevention and Lifestyle Changes section in this report.]
Treatment of Anemia
Blood transfusions are given for suddenly worsening anemia. However, transfusions can increase the risk for infections and cause a build-up of iron in the blood. [For more information, see "Transfusion Therapy" in Treatment section of this report.]
Folic acid and possibly iron supplements are often given. However, patients who are given multiple transfusions should avoid iron supplements. Also, folic acid can mask pernicious anemia, which is caused by deficiency of vitamin B12.
Treatment of Kidney Complications
Kidney damage in patients with sickle cell disease can cause bleeding into the urine. Mild episodes can usually be treated with bed rest and fluids. Severe bleeding may require transfusions.
Treatment of Priapism
Priapism causes prolonged and painful erections that can last from several hours to days. It is best to treat this problem within 12 hours. Relief within 36 hours is important to avoid permanent erectile dysfunction. Pain relief and intravenous fluids are the initial steps. Drugs used to prevent priapism include terbutaline and phenylephrine, which help restrict blood flow to the penis. A surgical procedure that implants a shunt to redirect blood flow is sometimes performed.
Treatment of Acute Splenic Sequestration (Damaged Spleen)
The spleen is often removed (splenectomy) in children who have one or two acute splenic sequestration crises. Transfusion therapy is an alternative for preventing acute splenic sequestration in high-risk patients.
Treatment of Leg Ulcers
Leg ulcers are difficult to treat. Simple treatment with a moist dressing usually provides the best results. To treat mild ulcers, gently wash the leg with cotton gauze soaked in mild soap or a solution of one tablespoon of household bleach to one gallon of water. A dressing soaked in diluted white vinegar may be applied every 3 - 4 hours.
More severe ulcers require debridement, which is the removal of injured tissue until only healthy tissue remains. Debridement may be accomplished using chemical (enzymes), surgical, or mechanical (irrigation) means. Hydrogels are helpful in healing ulcers and are noninvasive and soothing. Topical antibiotics, saline or zinc oxide dressings, or cocoa butter or oil are also used depending on severity. The leg should be elevated. Bed rest for a week or more is sometimes required for severe ulcers. Skin grafts and transfusions may be helpful in extreme cases.
Treatment of Sickle Cell Disease During Pregnancy
Women who are pregnant should be treated at a high-risk clinic. They should take folic acid in addition to multivitamins and iron. Standard treatment is given for sickle cell crises, which may occur more frequently during pregnancy. However, certain drugs (such as hydroxyurea) should not be taken during pregnancy. The benefits of transfusions to prevent crises during pregnancy are not yet clear and doctors recommend them only for women who experience frequent complications during pregnancy.
Prevention and Lifestyle Changes
General Precautions
To prevent or reduce the severity of long-term complications of sickle cell disease, several precautions may be helpful:
- Have regular physical examinations every 3 - 6 months.
- Have periodic and careful eye examinations.
- Have sufficient rest, warmth, and increased fluid intake. (These are critical precautions for reducing oxygen loss and the risk for dehydration.)
- Avoid situations, such as crowds, that increase risk for infections.
- Avoid excessive demands on the body that increase oxygen needs (such as physical overexertion and stress). Low impact exercise (such as leg lifts and light weights) may be useful and safe for maintaining strength, particularly in the legs and hips, but patients should consult their doctor before starting any exercise program.
- Avoid high altitudes if possible. If flying is necessary, be sure that the airline can provide oxygen.
- Do not smoke, and avoid exposure to second-hand smoke. Both active and passive smoking may promote acute chest syndrome in patients with sickle cell disease.
Preventing Infections
Vaccinations. Everyone with sickle cell disease should have complete regular immunizations against all common infections. Children should have all routine childhood vaccinations. The following are important vaccinations for everyone with sickle cell disease:
- Pneumococcal vaccines. All sickle cell patients should be vaccinated with the pneumococcal vaccine. There are two types of pneumococcal vaccines; the choice between them depends on the age of the patient. Infants and children less than 2 years of age should receive 4 doses of the pneumococcal conjugated vaccine (Prevnar) between 2 - 15 months of age. The pneumococcal polysaccharide vaccine should be administered at age 2 years or older, repeated after 3 - 5 years for patients younger than age 10, or in 5 years for patients older than age 10.
- Vaccination against Haemophilus influenza, the major cause of meningitis in unimmunized children, starting at age 2 months.
- Influenza vaccines ("flu shots") should be given every winter, starting at age 6 months.
- Meningococcal vaccination for patients age 2 and older.
- Hepatitis B vaccine. All children should receive this vaccine.
Tuberculosis skin testing should be performed every year except in patients who have tested positive in the past.
Antibiotics. In addition to regular immunizations, preventive (prophylactic) antibiotics are the best approach for protection against pneumonia and other serious infections among children with sickle cell disease. Babies diagnosed with sickle cell are given daily antibiotics, starting at 2 months of age and continuing through 5 years of age. Penicillin is usually the antibiotic given, unless a child is allergic to it.
Nutrition and Dietary Supplements
Foods. Good nutrition, while essential for anyone, is critical for patients with sickle cell disease. Some dietary recommendations include:
- Fluids are extremely important. The patient should drink as much water as possible each day to prevent dehydration.
- Diet should provide adequate calories, protein, fats, and vitamins and minerals. Patients and families should discuss vitamin and mineral supplements with their doctors and nurses.
- Some studies suggest that omega-three fatty acids, found in fish and soybean oil as well as dietary supplements, might make red blood cell membranes less fragile and possibly less likely to sickle, although no studies have proven this definitively.
Vitamins. Patients should take daily folic acid and vitamin B12 and B6 supplements. Vitamin B6 may have specific anti-sickling properties. Some doctors recommend 1 mg folic acid, 6 microgram vitamin B12, and 6 mg vitamin B6. Foods containing one or all of these vitamins include meats, oily fish, poultry, whole grains, dried fortified cereals, soybeans, avocados, baked potatoes with skins, watermelon, plantains, bananas, peanuts, and brewer's yeast. Of note, folic acid can mask pernicious anemia, which is caused by deficiency of vitamin B12 and is more common in African-Americans than other populations.
Note on Iron. Although sickle cell disease is often referred to as anemia, patients who receive multiple blood transfusions should avoid iron supplements or iron-rich foods, which increase the risk for iron overload.
Psychosocial Support
Sickle cell disease presents great emotional challenges for patients and their families. For the family, nothing is more heartbreaking than watching their child endure extreme pain and life-threatening medical conditions. The patient endures not only the pain itself but also the stress of not knowing when a sickle cell crisis will occur. They also have to struggle with lost time and social isolation at school and work, as well as fear of death.
Any chronic illness places stress on the patient and family, but sickle cell patients and caregivers often face particular obstacles in finding psychological support for the disease. Communities in which many sickle cell patients live may lack services that can meet their needs, and professionals who work in their medical facilities are often overworked. In a study comparing patients with different kinds of long-term illnesses, those with sickle cell disease gave the lowest scores to their doctors and other professional caregivers for compassion, and were least satisfied with their medical care.
It is very important for patients and their caregivers to find emotional and psychological support. The following are some measures that may help in dealing with this disease:
- Stress Reduction. Stress reduction techniques and relaxation methods appear to be helpful. Breathing and mediation techniques may be very helpful.
- Cognitive-Behavioral Therapy. Studies suggest that cognitive behavioral therapies that teach coping skills can result in less negative thinking and possibly less pain. Coping skills can help the patient's ability to manage symptoms such as pain.
- Support Associations. Support groups and on-line support communities can offer valuable advice and advocacy for patients and their families.
Resources
- www.sicklecelldisease.org -- Sickle Cell Disease Association of America
- www.nhlbi.nih.gov -- National Heart, Lung, and Blood Institute (NHLBI)
- www.sicklecellsociety.org -- Sickle Cell Society (UK)
- http://scinfo.org-- Sickle Cell Information Center
- www.clinicaltrials.gov -- Find clinical trials
References
Abboud MR. Hematopoietic Stem-cell transplantation for adults with sickle cell disease. N Engl J Med. 2009 Dec 10;361(24):2380-2381.
Adams RJ, Brambilla D; Optimizing Primary Stroke Prevention in Sickle Cell Anemia (STOP 2) Trial Investigators. Discontinuing prophylactic transfusions used to prevent stroke in sickle cell disease. N Engl J Med. 2005 Dec 29;353(26):2769-78.
Brawley OW, Cornelius LJ, Edwards LR, Gamble VN, Green BL, Inturrisi C, et al. National Institutes of Health Consensus Development Conference statement: hydroxyurea treatment for sickle cell disease. Ann Intern Med. 2008 Jun 17;148(12):932-8. Epub 2008 May 5.
Caboot JB, Allen JL. Pulmonary complications of sickle cell disease in children. Curr Opin Pediatr. 2008 Jun;20(3):279-87.
de Montalembert M. Management of sickle cell disease. BMJ. 2008 Sep 8;337:a1397. doi: 10.1136/bmj.a1397.
Dunlop RJ, Bennett KC. Pain management for sickle cell disease. Cochrane Database Syst Rev. 2006 Apr 19;(2):CD003350.
Geller AK, O'Connor MK. The sickle cell crisis: a dilemma in pain relief. Mayo Clin Proc. 2008 Mar;83(3):320-3.
Gladwin MT, Vichinsky E. Pulmonary complications of sickle cell disease. N Engl J Med. 2008 Nov 20;359(21):2254-65.
Gladwin MT, Kato GJ, Weiner D, Onyekwere OC, Dampier C, Hsu L, et al. Nitric oxide for inhalation in the acute treatment of sickle cell pain crisis: a randomized controlled trial. JAMA. 2011 Mar 2;305(9):893-902.
Hsieh MM, Kang EM, Fitzhugh CD, Link MB, Bolan CD, Kurlander R, et al. Allogeneic hematopoietic stem-cell transplantation for sickle cell disease. N Engl J Med. 2009 Dec 10;361(24):2309-2317.
Lanzkron S, Strouse JJ, Wilson R, Beach MC, Haywood C, Park H, et al. Systematic review: Hydroxyurea for the treatment of adults with sickle cell disease. Ann Intern Med. 2008 Jun 17;148(12):939-55. Epub 2008 May 5.
Lee MT, Piomelli S, Granger S, et al. Stroke Prevention Trial in Sickle Cell Anemia (STOP): extended follow-up and final results. Blood. 2006 Aug 1;108(3):847-52.
Platt OS. Hydroxyurea for the treatment of sickle cell anemia. N Engl J Med. 2008 Mar 27;358(13):1362-9.
Rees DC, Williams TN, Gladwin MT. Sickle-cell disease. Lancet. 2010 Dec 11;376(9757):2018-31. Epub 2010 Dec 3.
Roach ES, Golomb MR, Adams R, Biller J, Daniels S, Deveber G, et al. Management of stroke in infants and children: a scientific statement from a Special Writing Group of the American Heart Association Stroke Council and the Council on Cardiovascular Disease in the Young. Stroke. 2008 Sep;39(9):2644-91. Epub 2008 Jul 17.
Saunthararajah Y, Vichinsky EP. Sickle cell disease: clinical features and management. In: Hoffman R, Benz EJ, Shattil SS, et al, eds. Hematology: Basic Principles and Practice. 5th ed. Philadelphia, Pa: Elsevier Churchill Livingstone; 2008:chap 43.
Steinberg MH. In the clinic. Sickle cell disease. Ann Intern Med. 2011 Sep 6;155(5):ITC31-15; quiz ITC316.
Strouse JJ, Lanzkron S, Beach MC, Haywood C, Park H, Witkop C, et al. Hydroxyurea for sickle cell disease: a systematic review for efficacy and toxicity in children. Pediatrics. 2008 Dec;122(6):1332-42.
Tsaras G, Owusu-Ansah A, Boateng FO, Amoateng-Adjepong Y. Complications associated with sickle cell trait: a brief narrative review. Am J Med. 2009 Jun;122(6):507-12. Epub 2009 Apr 24.
U.S. Preventive Services Task Force. Screening for Sickle Cell Disease in Newborns: U.S. Preventive Services Task Force Recommendation Statement. AHRQ Publication No. 07-05104-EF-2, September 2007. Agency for Healthcare Research and Quality, Rockville, MD.
Wang WC, Ware RE, Miller ST, Iyer RV, Casella JF, Minniti CP, et al. Hydroxycarbamide in very young children with sickle-cell anaemia: a multicentre, randomised, controlled trial (BABY HUG). Lancet. 2011 May 14;377(9778):1663-72.
|
Review Date:
2/7/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |










